Of all fungal diseases, the most common are mycoses (fungal lesions) of the skin of the feet. They are also called ringworm or athlete's foot. Approximately 30% of the population has problems with diseases of a fungal nature. Almost half of the patients never go to the doctor with them, spreading the fungus among their loved ones. Microscopic pathogens affect the dermis (skin) or nails. In the latter case, they are talking about onychomycosis.
Why are the feet most commonly affected?
Various fungi are always present on the skin. Their reproduction is hindered by beneficial bacteria and skin secrets. In the event of a violation in the work of immunity, a change in the composition of the microflora of the skin, there is a favorable time for fungi - they can reproduce freely. The gateway to infection can serve as regular damage:
- scratches;
- cracks;
- chafing.
Another cause of mycosis is endocrine disorders. In case of disturbances in the work of the endocrine glands, not only the balance of hormones changes, but also the work of the entire organism. Including, the composition of skin secretions changes, due to which they lose their bactericidal properties. Fungi can feed on them, which also promotes reproduction.
Other factors also contribute to the weakening of protective forces:
- alimentary exhaustion (malnutrition);
- avitaminosis;
- excessive physical and psycho-emotional stress;
- concussions;
- regular stress.
These are all non-specific causes of fungal skin lesions. Because of them, mycoses of the feet, smooth skin on the body or mucous membranes can develop.
In addition, there are special types of fungi (genus Trichophyton or Microsporum) - pathogenic (pathogenic). In contact with the skin or on its surface, they cause disease. In the case of the feet, the disease is called rubromycosis. On the body, these pathogens form specific spots - ringworm. You can get infected from a person or an animal.
The skin of the feet is a special place for fungi. There are always many keratinized cells. Microbes are used as accommodation and food. "Understood" fungi contribute to sweaty feet. In closed shoes, a moist environment rich in nutrients forms on the feet - the "dream" of every fungus. If a person neglects foot hygiene, does not dry and disinfect the shoes, the infection first multiplies in them, and then passes to the "owner's" feet. Poor hygiene products, dryness, synthetic socks also contribute to the spread of fungal infection.
Signs of fungus, visible visually
Treatment of dermatomycosis is easier, the earlier the disease is diagnosed. In advanced cases, the therapy is long-term, involves taking pills and using external means. In the initial stages of mycosis, fats can be avoided. It is important to know how to recognize the early symptoms of fungus in order to see a doctor in time.
How the fungus looks depends on the form of mycosis. Fungal infection of the feet can occur in 3 different variations, as well as in a mixed form - when the signs of the three main varieties are simultaneously present on the feet.
Intertriginous form

A type of tinea pedis that primarily affects the skin between the toes. The first symptom of the disease is the appearance of a painful crack between the 3rd and 4th or 4th and 5th rings of the foot. The damage is small, but it causes inconvenience when washing your feet and walking.
If you carefully examine the wound, a whitish fringe can be seen around it (example in the photo). This is what the edges of the skin around a crack that has peeled off look like. The wound may itch, ooze, enlarge, or vice versa - occasionally heal and then reappear.
In some cases, the crack heals, but the skin is still lost, hyperkeratosis develops (thickening of the dermis), corns and blisters appear. In advanced intertriginous form, the cracks become larger (example in the photo), appear between other fingers, the skin is constantly moistened. It is difficult for the patient to move, to wear any kind of footwear.

As this shape progresses, the crack increases in size. Similar signs appear on the other foot. Thick and large layers of skin peel off around the wound. The other (hooked) end is not rejected and attempts to remove the keratinized part with the fingers end in additional damage to the foot.
This type of foot fungus is the most common. At first, the manifestation of the pathology is not accompanied by any symptoms. As a rule, the infection develops between the 3rd and 4th finger and does not change the color and structure of the skin until a certain moment. After that, moist cracks and layers of skin appear.
The foot itself remains unharmed, however, if it is affected by the fungus, the feet may sweat more than usual. Therapy of the fungus of the intertriginous form is characterized by medium complexity.
Dyshidrotic form

In this form, the first signs of fungus on the skin are blisters on the arch of the foot. Most often - near the heel. The surface becomes dry, deep seals (like lumps) appear on it. Later, they noticeably rise above the level of the skin, because they are filled with liquid. Vesicles (vesicles) are usually small - from 2 to 5 mm in diameter. They can merge, forming larger - bullae. Other symptoms include pain and itching around the rash.
The progression of the dyshidrotic form of mycosis is manifested by the bursting of blisters. Small or large erosions occur in their place. They often become infected with bacteria and start to boil. Erosions do not heal for a long time, making walking painful. In some cases, erosion disappears, and dryness appears in their place.
squamous form

As the disease progresses, severe hyperkeratosis develops on the feet. The size and number of cracks increases. The biggest ones can bleed. Such damages are a way for other pathogenic microbes to invade the body. Because of this, the wounds periodically become inflamed and can become abscessed. The most common form of foot fungus is manifested by increased dryness of the skin on the plantar part of the limb. This can mean a recent approach of the fungus, or vice versa - be the result of the development of other forms.
On the arch of the foot and in the center, the dermis becomes dry, thin, shiny, covered with a network of furrows. In the area of the toes and heels, hyperkeratosis is observed - rapid keratinization, in which dead particles do not have time to exfoliate. Blisters or corns form on the front part of the foot. There are small cracks on the heels. The entire surface is rough due to pronounced peeling. The patient may feel itching. With prolonged development of mycosis, this symptom is absent.
Fungus on the legs can be determined by excessive dryness, unpleasant odor, itching and constant peeling of the skin.
Onychomycosis
Onychomycosis is a type of foot (or palm) fungus that affects the appendages of the skin - the nails. Nail fungus can be caused by the same pathogens that cause mycosis of the skin. You get infected with mold and other types of mono fungi in the manicure room, on the beach, when trying on new shoes with bare feet, when going to the sauna or the pool. An ingrown toenail can be a contributing factor. The thumb is most often affected.
When it hits the nail plate, the fungus begins to divide. It penetrates deep into the nail, spreads over its area. The first signs by which you can determine nail fungus are the loss of shine, the appearance of spots (white, yellow, brown, greenish), a change in the shape of the nail plate.
As the disease progresses, the structure of the nail changes in the discoloration zone (it thickens, becomes bumpy, loose).
Running toenail fungus looks like thick yellow growths. Affected nail plates are difficult to care for. Before each trimming, you must make warm baths for the feet. After contact with water, nails become softer and easier to remove with manicure tools.
If the nail fungus is not treated, onycholysis begins - the plate completely or partially peels off. After removing its remains, the nail does not always grow back. Sometimes the separation process ends with the complete loss of the nail.
General principles of treatment
Fungi on the feet are treated with ointments, creams, solutions, and special varnishes. In parallel, the patient is prescribed antifungal tablets.
Careful foot hygiene, weekly cutting and sawing of the damaged part are shown for the entire treatment period. Every day, the patient must remove the keratinized layer of cells from the surface of the feet using a pedicure file.
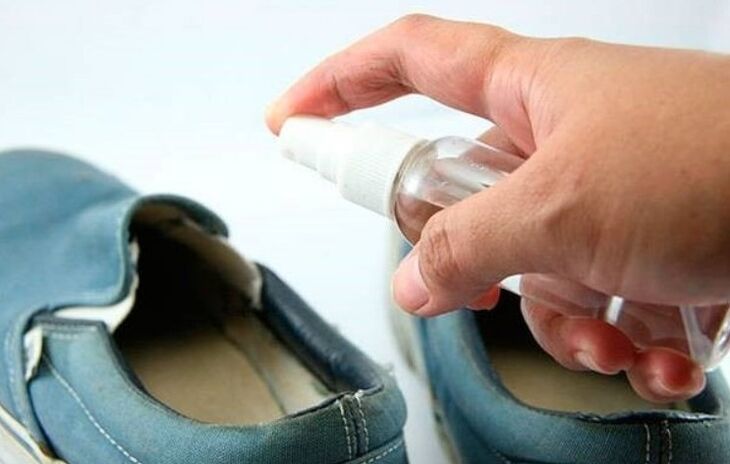
It is also important to take good care of your shoes - treat them with antifungal drugs or disinfectants. Shoes are dried and aired outdoors daily.
External resources
In the initial stages of foot fungus, only ointment or cream is prescribed. Cream and other medicines are prescribed for treatment. They are applied to the skin 1-2 times a day, after thoroughly washing the feet with simple soap. Before using the cream, it is important to dry the feet completely. Do not apply the medicine to wet skin. After the treatment, the patient should wear cotton socks.
Tablets
It is impossible to treat the fungus on your own with tablets. All drugs have a negative effect on the work of the liver and kidneys, and have a number of contraindications. Before prescribing a course of antifungal tablets, the specialist will recommend taking a general and biochemical blood test, which can be used to assess the condition of vital organs.
Nail preparations
Useful in the treatment of onychomycosis and foot fungus. In the first case, they are used to remove the affected part of the nail, in the second - to prevent infection of the nail plates with fungi.
It is most convenient to treat yourself with varnishes - they are applied to the nails 1-2 times a week. The most favorable medicines for nail fungus are solutions, applied to the nails 2 times a day until complete recovery. Special gels are popular. They visually improve the condition of the affected nails, along the way they stop the reproduction of fungi. Ointments are also prescribed for onychomycosis. They are applied in a thick layer to the affected plates, covered with a bandage, and kept like that until the product is completely absorbed. The treatment is repeated twice a day.
Preventing foot fungus is much easier than treating it. To do this, you must lead a healthy lifestyle, bring your own slippers to the pool and sauna, wash and air your shoes regularly, wear socks made from natural fabrics and use anti-perspirant products. Along with regular visits to "wet" institutions, antifungal creams should be used prophylactically - treat the skin of the feet 1-2 times a week.
















